The PRP Controversy: When Your Hair & Patience Are Thinning
July 18, 2019 | cosmetic, hair restoration, prp
In May, Health Canada released a position paper on "Autologous Cell Therapy Products" stating that the risks associated with these treatments pose a risk to the public. An article subsequently published in the Globe and Mail in July described a number of clinics that were forced to stop offering these therapies, claiming that the clinics were “peddling misinformation to sell expensive [...] treatments that don’t live up to the marketing hype”. The author cited a paper published in the New England Journal of Medicine where stem cell injections caused blindness in 3 patients. She failed to mention that this was a trial where patients were literally injected into their eyeballs with processed stem cells. Not exactly the same as platelet-rich plasma (PRP) for the scalp or skin, but nonetheless, the lines were blurred.
Whereas the Health Canada paper was clear that they wanted to engage collaboration for further research, the Globe article has spawned a public outcry, leading many patients to question whether platelet-rich plasma is right or even safe for them.
Let’s set the record straight, shall we? PRP does not equal “stem cell”. PRP has been around for decades with a multitude of applications in medicine. PRP is supported by large-scale clinical trials. PRP is safe for injection in skin and scalp. So why the pushback? We think the answer is a lack of public awareness into what PRP is and what PRP does. There is also a significant discrepancy in how PRP is processed, injected and its resultant effectiveness. So today, let’s talk everything PRP for cosmetic purposes.
The first description of PRP in medicine was in 1990 when researchers observed a 50% reduction in healing time in chronic wounds. Similarly, growth factors from PRP yielded promising results in the field of orthopedics where biologic fixation of implants was seen. Since that time, over 15,000 articles have been published on PRP’s uses in joint surgery, oral surgery, plastic surgery, dermatology and gynecology amongst others.
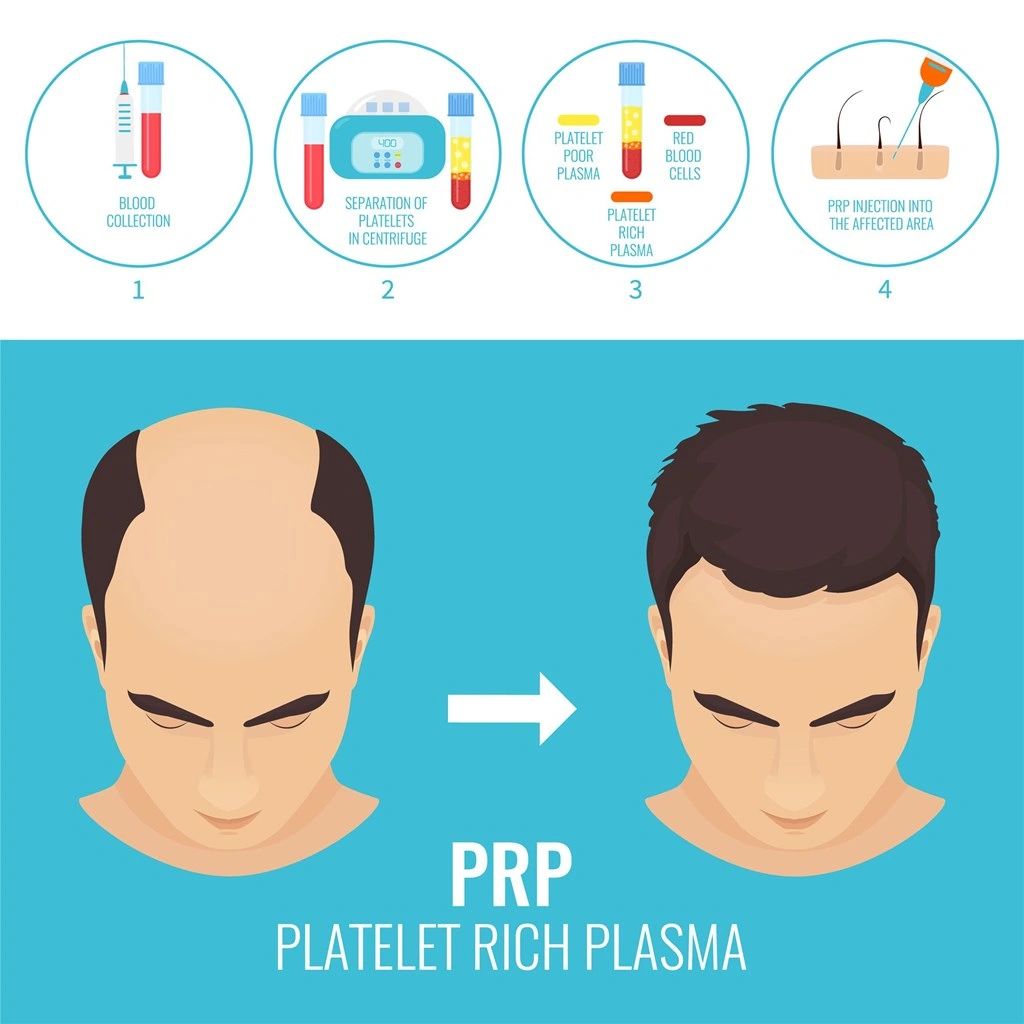
But what is PRP? Platelet-rich plasma comes from our bone marrow and is a component of our blood which contains water, proteins, albumin and clotting factors. Platelets are responsible for wound healing as they stick to injury sites on our body, aggregate together to form a “plug” and then release substances to trigger the next steps. Additionally, growth factors contained within platelets like platelet-derived growth factor (PDGF) attract other cells involved in healing to promote a better blood supply and healing of the skin.
Platelet-rich plasma is an autogenous material, meaning it comes from you, the body recognizes it as you and it has positive effects only on you. The processing of PRP is simply to increase the concentration of the growth-factor rich component of blood, between 3- and 27-fold depending on the technology used. There are principally four product categories obtained after processing: pure platelet rich plasma (P-PRP), leukocyte and platelet rich plasma (L-PRP), pure platelet rich fibrin (P-PRF), leukocyte and platelet rich fibrin (L-PRF). Some in the media may interchange the terms “stem cell” and “PRP” liberally, not recognizing the difference. Stem cells have are pluripotent or multipotent cells in our body (usually from blood, bone marrow or fat) that are processed with chemical reactions to return them to their most primitive state, able to then transform into any cell. Stem cells are heavily regulated because of the many processing steps needed. PRP is not a stem cell. PRP is simply an existing component of blood that is isolated from the rest (i.e. red and white blood cells) and may actually stimulate our own native stem cells (specifically mesenchymal stem cells) to start working better.
PRP was popularized in the cosmetic world by the Kardashians undergoing “Vampire Facelifts”, a procedure in which microneedling of the skin was then coated with the healing properties of PRP. A recent study examined 108 articles and concluded that PRP does play a role in facial rejuvenation, specifically due to its ability to promote tissue regeneration and revascularization. This same thinking went into the decision to introduce PRP for hair restoration. Androgenic alopecia is the result of an increased level of an enzyme called 5-alpha-reductase that converts testosterone to dihydrotestosterone (DHT). As a result, the growth phase of our hair (anagen) shortens and the resting phase (telogen) lengthens, leading to miniaturization of our hair follicles. Using therapies to target cellular proliferation and differentiation to promote a longer growth phase would therefore be quite useful. PRP has been shown to stimulate hair growth by inducing follicular stem cell differentiation, prolonging anagen and prolonging cell survival. It also increases the surrounding blood supply through increases in growth factors VEGF and the aforementioned PDGF.
Since the early 2000s, PRP has been used for male and female pattern baldness. The first study to look at wound healing with PRP after hair transplant was done in 2007 by Perez-Meza et al. In it, they used histological and cellular data from multiple biopsies taken over time to show that growth factors play an essential role in graft healing and that maintaining a healthy blood supply to the scalp should increase survival rate. PRP was initially used during hair transplantation for support of the grafts, but has since been applied de novo in non-transplanted patients looking to avoid surgical intervention. In the last 15 years, 141 studies have been published on PRP and hair. Many have shown PRP to increase the mean number of hairs and hair thickness in tested subjects up to 30%.
So why is Health Canada raising issues with PRP? There are many reports of the different processes used to concentrate it and the resulting cellular composition of PRP. Some work, some don’t. Studies have shown that there is an optimal concentration for platelets in PRP (1.5 M/microliter) afterwhich the therapy has the reverse effect. Indeed, there are clinics around the country that do not adhere to the sterility principles one would find in a medical clinic and do have greater rates of infection. Health Canada claims that the “prolonged exposure” carries long-term risks such as viral or bacterial infection; however, some studies show that PRP exerts its effects within the first hour after injection and is washed out shortly thereafter. In fact, newer research has gone into finding other substances to combine PRP with to ensure it sticks around for longer. Additionally, there are different ways that the product is injected into the scalp (i.e. mesoinjection, gun, needle, microneedle, etc...). More important than anything else, patient selection is the most important predictor of success. PRP works to reverse miniaturization - if you have no more follicles, you will not grow hair! Be wary of providers who tell you that a bald scalp can be cured with PRP. All of these variables add up to uncertainty when seeking a provider for PRP.
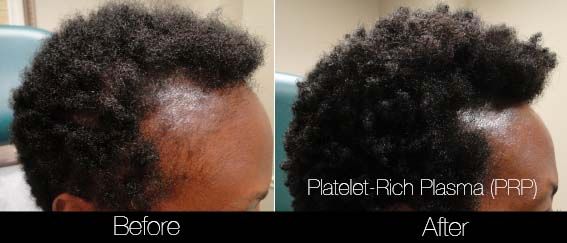
Ultimately, Health Canada is doing its due diligence to ensure safety and standardization in the market. Questioning the efficacy of PRP for non-invasive procedures like skin and hair may prove fruitless, but it certainly forces providers to look critically at outcomes to ensure patient satisfaction. As my mentor Dr. Mulholland says, “a picture is worth a thousand words, but a 'before and after' like a mute button”. Enough talking, see for yourself...